This is an online e logbook to discuss our patients deidentified health data shared after taking her/guardian's signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs
A 65 year old male resident of suryapet farmer by occupation, presented to the opd with complains of swelling of the legs and shortness of breath since 7 days
Patient complains of dark stools since 4 days
Patient was apparently asymptomatic 7 days before the date of admission .Then he developed bipedal edema and shortness of breath from 7 days
Dark coloured stools since 4 days
There is no pain in legs while walking
Patient visited local hospital in miryalguda where he was diagnosed as having renal caliculi
Then he visited our hospital
Patient is having anemia
He is suggested to get a blood transfusion for anemia
He is having constipation from last 2 days
Daily routine before illness:-
Patient used to get up at 6 am he used to go to his field taking the breakfast and lunch with him
He used to have his breakfast at 7 am
He used to do ploughing work in his field till 6 pm
Having lunch in between 12:30- 1pm
He used to come home at 6 pm
He used to have his dinner at 7pm
Patient used to go to bed at 7:30 pm
Daily routine after illness:-
Patient gets up at 6 am
He sits idle he cant walk due to his increased shortness of breath
He has his breakfast at 8 am
He has his lunch at 1 pm
He has his dinner at 8 pm
Past history:
Patient is diabetic from 10 years
No h/o hypertension,tuberculosis,asthma,epilepsy, cerebrovascular accident
Patient has h/o CAD
Patient has history of renal stones
Patient has undergone eye surgery on right side 5 years back
Personal history:
Diet:Mixed
Apetite: loss of appetite from 1 week
Addictions: occasionally alcoholic he consumes 90 ml of whisky
Non smoker
Sleep: Adequate
Bowel&Bladder movements:Normal
Family history:
No h/o similar illness in the family
Medical history:
Patient is not allergic to any drug
Treatment history:
Patient has undergone surgery of right eye
General examination:
Patient was conscious, coherent and cooperative and well oriented with time and person
Gait: Normal
Built:poorly built
Nourishment:
Pallor:present
Clubbing:no clubbing
Icterus:no icterus
Lymphadenopathy:no lymphadenopathy
Cyanosis:no cyanosis
Systemic examination:
Vitals
Temperature:afebrile
Respiratory rate:16 cpm
Pulse rate:77 bpm
Bp:120/60 mm of Hg
SYSTEMIC EXAMINATION:
CVS:S1S2+
No murmurs
JVP:Normal
Apex:6th ICS
CNS:NAD
R/S:BAE+
NVBS+
P/A:Abdomen distended
Umbilicus everted
No fluid thrill
Soft,BS+
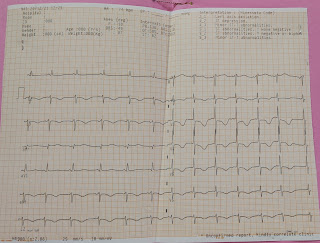
INVESTIGATIONS:
Treatment:
1.Fluid restriction <1.5 l/day
2.Salt restriction <2.5 gm/day
3.INJ LASIX 40 mg iv/BD (If sbp> or equal to 110 mm Hg
4.Tab LORYL -M2 PO/BD
5.Tab Carbamazepine 200 mg PO/BD
6.Monitor vitals 4th hrly
7.GRBS-6th hrly
8.I/O- CHARTIN G
9.Daily weight Monitoring
Tab.Ecospirin-AV(75/20) PO/OD
















Comments
Post a Comment